Racing to the rescue: Mercedes innovation that helped fight Covid
When Covid struck there was a critical shortage of NHS ventilators. As a new book explains, an F1 team swung into action to design and build a device in record time – and saved thousands of lives
Professor Becky Shipley walked into the soft, comfortable interior of the staff common room at University College London (UCL) and sank into one of its deep crimson leather sofas. It was Tuesday evening, March 17, 2020. Outside, the leafy squares of Bloomsbury were placid in the evening air, the streets empty and eerily quiet even for the renowned peace of this oasis in the heart of London. The Covid-19 virus had spread across the globe, migrating in bodies of travellers, unknowing vectors who took a modern plague across borders and continents. The virus made you struggle for breath; the worst-hit couldn’t breathe at all. Gradually, the world was waking to a bitter truth. It faced a global pandemic in which millions would die.
A few days earlier, the UK government had launched its ‘Ventilator Challenge’. The UK’s hospitals had fewer than 6000 ventilators available at the start of the coronavirus pandemic and, after a rush to get more, it still only had 8175; to meet the expected worst-case scenario for Covid-19, it needed 30,000 in a matter of weeks. The scramble had been unprecedented. The NHS had even taken functional ventilators used as props on the TV medical drama Holby City.
The Ventilator Challenge was recruiting groups across the UK’s manufacturing sector, asking them to stop business as usual and start saving lives. That Sunday, Shipley had been called by Professor Cathy Holloway, who had been asked to lead one of the Government’s low-cost ventilator ‘design sprints’. Would Shipley like to run the project with her?

Professors Becky Shipley and Mervyn Singer from UCL were involved with the ventilator scheme from the start
Shipley declined.
A bioengineer, Shipley had been raised in nearby Buckinghamshire before studying mathematics at the University of Oxford. Now at UCL, she was director of the university’s Institute of Healthcare Engineering. And she knew the Government’s plan wouldn’t work.
Instead, she had called an informal meeting in the common room. Joining her on the sofa was Mervyn Singer, professor of intensive care medicine at University College Hospital (UCLH) across the road. Sitting opposite was Tim Baker, a UCL professor of mechanical engineering. Rather than come up with new ventilator designs, the trio realised UK hospitals would be overwhelmed in weeks unless they could keep people off ventilators. Singer even had an idea for a machine that could do it. The group just needed advice on how to make the thousands of units necessary before the pandemic hit its peak.

Covid struck F1 during the weekend of the Australian Grand Prix in March 2020
Now Baker took the lead. Before joining UCL, he had been part of several Formula 1 teams, as well as teams that won their class at the Le Mans 24 Hours and the World Rallycross Championship. Picking up the phone, he rang an old friend and colleague, Ben Hodgkinson, the head of mechanical engineering at Mercedes-AMG High Performance Powertrains, responsible for the power units for the Mercedes, Williams and Racing Point (now Aston Martin) teams. Baker told Hodgkinson their idea and asked if he could take a sabbatical for a few days, come down to London and consult on their project. Motor sport engineers, after all, were used to pulling off the impossible.
Hodgkinson took the plan to his boss, managing director Andy Cowell. His response to the UCL professors was even more ambitious: “Do not hesitate to call upon the full might of what we can do.” UCL and Formula 1’s leading engine manufacturer were about to pull off one of the most astonishing, life-saving feats in engineering history.
Formula 1 has a surprising connection with the NHS. For the past 20 years, F1 has been lending its expertise to doctors in all sorts of unlikely ways.

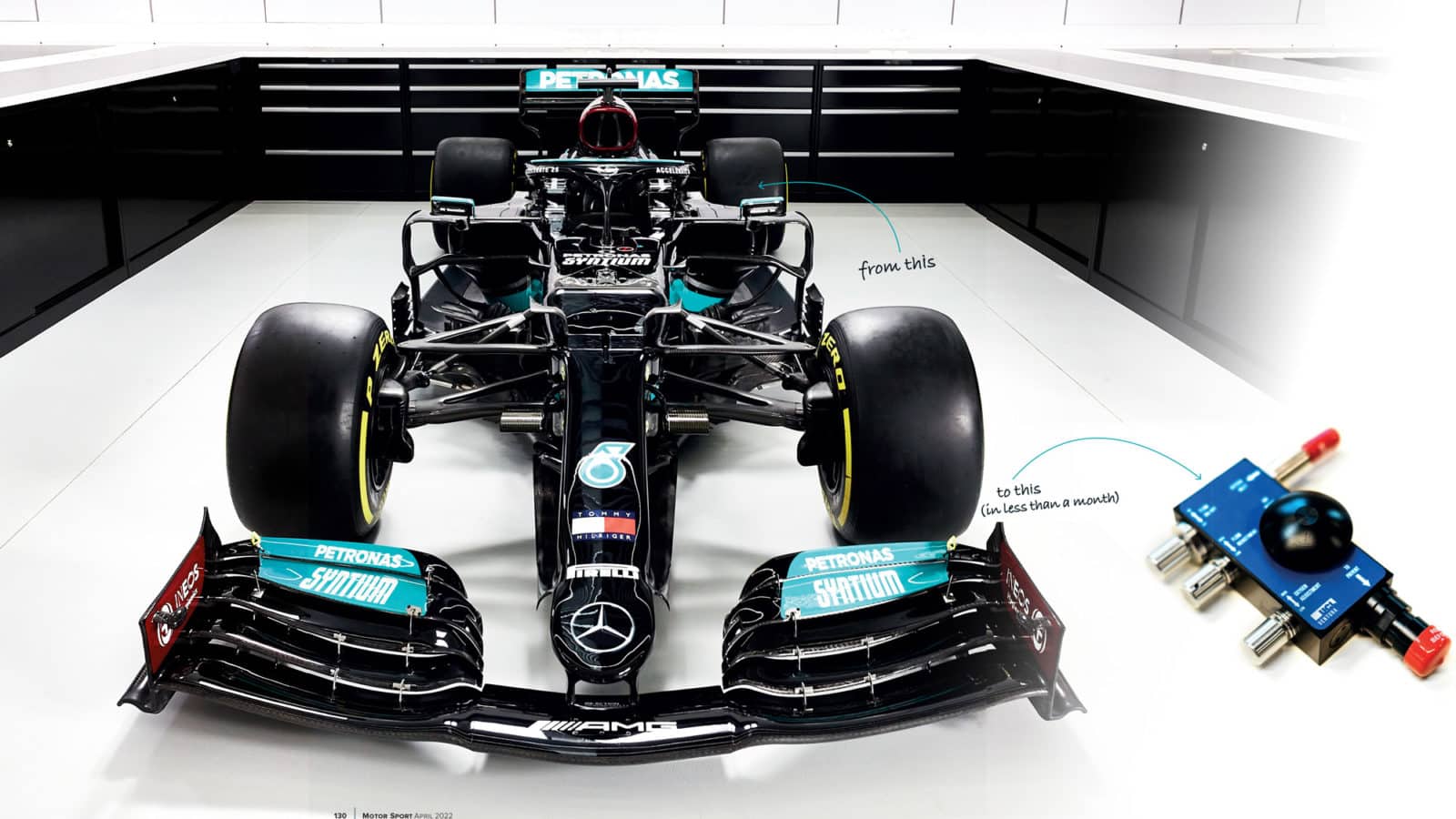
The factory of Mercedes AMG High Performance Powertrains switched from creating world-beating racing tech to life-saving ventilators
In 2003, paediatricians Allan Goldman and Martin Elliott were watching a grand prix after their shift at Great Ormond Street Hospital. Both realised there was a startling similarity between a pitstop and transferring a child after a successful operation to the intensive care unit. In hospitals, 70% of mistakes are usually breakdowns in communication – technical or information errors – and half occur at this ‘hand-off’, for example by transferring a patient before a bed is set up for them. Goldman wondered if his team could copy the balletic precision that makes a pitcrew able to change four tyres in less than three seconds.
Goldman asked McLaren to explain how it choreographed its pit moves, then headed to Maranello to witness the Ferrari mechanics in action. The lessons were obvious: strict, well-drilled routines practised to perfection and reviewed; each person with one task, working in calm silence rather than distracting noise; and a ‘lollipop man’ to co-ordinate the effort. The team sent Ferrari a tape of their own handover; the mechanics took notes, made suggestions, and sent them back. The Great Ormond Street surgical teams came up with new handover protocols. After two years, the surgeons published their results: technical errors had fallen by 42%, information errors by almost half. Operation Pitstop had been
a complete success.
Given F1’s pedigree in solving problems, it’s hardly surprising Baker knew the Mercedes team had the ability to help with the UCL plan – and it wasn’t as though they were busy. The Formula 1 season was on an unofficial hiatus. That weekend, the Mercedes team had been in Melbourne, Australia, preparing to defend both the constructors’ and drivers’ championship titles. But the race was abandoned due to Covid, joining the already cancelled Chinese Grand Prix. By the time Baker phoned Hodgkinson, it was apparent that there would be no racing until May at the earliest. The engines were off, the garages shut, the pitwall empty. Even so, Cowell’s unflinching response to the UCL professors was an astonishing commitment. This wasn’t about applying existing Formula 1 principles to another environment, or adapting existing technology for a greater purpose. He had just put the full strength of a Formula 1 team into making a healthcare device they’d never seen before, let alone used in racing.

With the 2020 season on hold, Mercedes’ expertise moved to the medical world
Heading down to London, Hodgkinson met the UCL and UCLH team, which handed him the device they had in mind. Immediately, Hodgkinson recognised the elegance of its simple design. It was valves. Hydraulics. Simple mechanics. It was just the kind of challenge his engineers would relish. He picked his best three and told them they had two hours to get to London.
A ventilator is basically a high-tech set of bellows that responds to a patient’s breathing, taking over and doing the hard work. The downside is that ventilators are big, complex and require specialist skills to design and make – particularly when it comes to their control mechanisms. “The idea that you could redesign and manufacture them at scale in weeks didn’t make much sense,” Shipley recalls.
Singer’s alternative was to use a continuous positive airway pressure, or CPAP, machine. Typically used to treat acute respiratory diseases, sleep apnoea, even snoring, a CPAP machine is simple to operate and patients only need to wear a tight mask for it to work. Rather than function like an artificial lung, a CPAP uses the venturi effect (fast-moving air sucks the air around it) to push gases through a series of valves and create a rapid air flow.

Niki Lauda, a non-executive chairman with Mercedes, helps celebrate a third consecutive constructor’s title in 2016. In 2020, a gathering like this would have been unthinkable
Unfortunately, there were not enough CPAP devices in the UK. UCLH Trust had just 12. The team knew the UK’s hospitals would need thousands if they were going to make a difference, and need them urgently. The team earmarked an existing device called WhisperFlow designed in the 1960s – one example of which Cowell had bought off Ebay (Mercedes’ operations manager was dispatched to pick it up from the seller’s doorstep and bring it back to the team factory at Brixworth, near Northampton, for analysis).
The task facing UCL – and Mercedes – was to take the WhisperFlow, reverse-engineer and copy it perfectly, design a new version, prove it was safe, get it signed off by regulators and go into full-scale production. It was a task that usually took a couple of years. The UCL team had to do it in less than four weeks. “We were a bit bonkers, really,” Shipley says.
In London, the team based itself at UCL’s MechSpace, with doctors, academics and engineers working together, and the Mercedes and UCL engineers renting nearby hotel rooms so they could toil into the night. In both London and Brixworth, the engineers began to reverse engineer the devices the old-fashioned way: by slicing them in half and poking about. From there, things became a little more high-tech. “Once we worked out the design, we redid it in 2D and 3D and ran materials characterisations,” Shipley says. “We did CT scans, then made a prototype.”
The group worked round the clock without a break, drafting drawings and coming up with new iterations. Hodgkinson had told his team to come to London without stopping at home, so the Mercedes engineers didn’t even have a change of clothes. “When it became clear it would be more than a couple of nights we’d need to stay, one of the university students was sent out to buy pants, toothbrushes and T-shirts,” Hodgkinson says. “The only shirts he could find were some pink ones with ‘Ventura’ written on them.” The emergency apparel quickly became the official team uniform, and the collaboration had a name: UCL-Ventura.
The work was intense. “I famously said, ‘This should take us four hours,’” Hodgkinson remembers. “It took us more like 40. We worked until 5am and then got up at 7am for three days in a row. I can honestly say, even in Formula 1, I’ve never worked that hard. In Formula 1, I manage my stress by telling myself, ‘It’s only racing cars.’ When you’re working on something that could potentially save lives, you don’t have that. I’ve never pushed myself so hard. We slept for seven hours in three days.”
Hodgkinson had set a marker to have a prototype under way within 24 hours of arriving at the MechSpace. In the end, the team missed the deadline by two hours. Three days later, the first devices were at the hospital, ready for testing by volunteers.

Manufactured at Mercedes’ Brixworth factory, the CPAP device has saved countless lives around the world – and blueprints are freely available online
“We started on Tuesday, Mercedes turned up on Wednesday and by Sunday we were at UCLH testing them on the wards,” Shipley recalls. It was one of the fastest turnarounds in medical history.
By now, the UK’s medical watchdog, the Medicines and Healthcare Products Regulatory Agency (MHRA), was aware of the project. “I remember emailing their chief executive, June Raine, at about 10pm – we’d been working for a whole day then, and it had become clear we could do this,” says Shipley. “She replied minutes later and we spoke to the MHRA the next day. From that day forth, we were in regular contact, so we had a real understanding of what we needed to do to proceed with approval.”
Even as the MHRA reviewed their take on the WhisperFlow device, UCL-Ventura were already working on a second version. Their prototype had been a carbon copy of the original but had little design flaws that irritated the Mercedes perfectionists. The engineers couldn’t resist the chance to tinker and make an even better CPAP machine and began to suggest improvements they could make to the machine’s assembly, including adding a single flap valve to cut down flow.
“Engineers are creative,” says Cowell. “On a simple task like copying, the creative genius gets frustrated and bubbles up in the odd area. Engineers will never just copy, they will always improve.” To test the breathing circuits, a new member of the team was brought in: a full-size male mannequin called ‘Ace’. The life-sized figure was soon recognised as a vital member of the Mercedes team and even got his own pink Ventura T-shirt. Elsewhere, Hodgkinson instructed his aero staff to run CFD simulations to analyse the oxygen flow through the device. “Two days after we got approval for the Mark I,” Shipley says, “we got the new version approved too.” The new design slashed the machine’s oxygen demands by 70%.
It was now March 29. The UCL-Ventura team had designed, tested and perfected two devices in 12 days. As the devices were backed by the MHRA, the Government didn’t hesitate to put in an order for 10,000 machines.
Mercedes now had an entirely new problem: how were they going to make them all in just two weeks? Then disaster struck. Hodgkinson caught Covid-19.

Putting in the hours: Ben Hodgkinson, head of mechanical engineering at Mercedes
With Hodgkinson out of action, colleague Pierre Godof, now Mercedes’ chief engineer on Formula E powertrains, took over. The task was monumental: Mercedes needed to move from making two engines a week to making thousands of CPAP devices a day. A few weeks earlier, most of the team had never even heard of a CPAP. “This is where Mercedes were just phenomenal,” says Shipley.
Instead of starting from scratch, Mercedes looked for a similar assembly line in their own factory that they could re-purpose. The closest thing they could find to a CPAP machine was a Formula 1 car’s fuel pump. Soon, they had copied the line across the factory, paying around £50,000 for new machine tools to allow the parts to be made.
By now the UK had entered lockdown, and the Mercedes factory had closed to all but essential workers. But, as news of the UCL-Ventura project spread, the team found itself inundated with colleagues volunteering to return. To speed up production even further, the UK’s Manufacturing Technology Centre provided the team with two automated guided vehicles (AGVs). These were driverless forklift robots, built to help shift parts around a factory. The AGVs were soon put to work, covering 12 miles a day to ensure the Mercedes production lines flowed. At first, the machines gave off a ‘wurp, wurp’ alarm as they trundled along. Within a day the engineers had hacked the robots, programming them to zoom about to The Imperial March from Star Wars. At their peak, the team’s 12 production lines were producing 1200 CPAP machines a day.
The 10,000th UCL-Ventura CPAP machine was delivered to the NHS on April 15, 2020. It had been just 30 days from when Baker, Singer and Shipley had met in the university’s staff common room. By the time the first wave of the pandemic hit its UK peak, machines built at Mercedes were available in more than 60 hospitals across the country. The team’s superhuman effort had saved countless lives.
The team won the 2020 Formula 1 constructors’ championship title and Lewis Hamilton claimed a seventh world title. But many of the team consider their delivery of the CPAP devices the real victory that year. “We’ll never, ever forget it,” says Cowell. “It’s a real privilege to work with people in this business. You don’t have to say anything. You just have to provide people the space, the tools, the direction, the target, and you can stand back and watch the magic happen.”
This is an edited version of a chapter taken from Racing Green: How Motorsport Science Can Save The World, by Kit Chapman. Published by Bloomsbury, £20
